INDIA'S FIGHT AGAINST TB: CHALLENGES AND STRATEGIES
INTRODUCTION:
- Tuberculosis (TB) is a severe infectious disease caused by the bacterium Mycobacterium tuberculosis, primarily affecting the lungs.
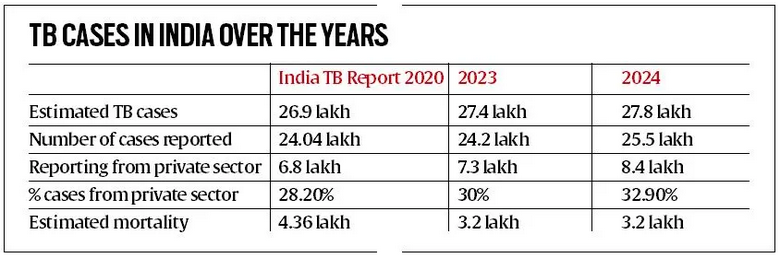
- Despite being curable, TB remains one of the top 10 causes of death worldwide and a significant public health challenge. India bears a disproportionate share of the global TB burden, accounting for over a quarter of the world’s cases.
- The World Health Organization (WHO) Global TB Report 2023 highlights that India had 25.1 lakh TB cases in 2023, showcasing strengthened case-finding efforts. However, the path toward TB elimination is fraught with challenges that need urgent and strategic intervention.
CHALLENGES HINDERING PROGRESS TOWARDS TB ELIMINATION IN INDIA:-
High Burden of Drug-Resistant TB (DR-TB):
- Challenge: Drug-resistant TB is a major obstacle to TB control efforts. The emergence of Multi-Drug-Resistant TB (MDR-TB) and Extensively Drug-Resistant TB (XDR-TB) complicates treatment and increases mortality rates.
- Example: India reported around 1.24 lakh DR-TB cases in 2023. The current treatment regimens are long, complex, and often lead to severe side effects like hearing loss and psychosis, resulting in poor patient compliance and treatmentout comes.
- Case Study: A study in Mumbai highlighted that only 60% of MDR-TB patients completed the lengthy treatment course due to severe side effects and economic hardships.
Diagnostic Delays and Missed Cases:
- Challenge: Delays in diagnosis due to inadequate screening methods and a lack of awareness lead to the continued transmission of TB within communities.
- Example: The National TB Prevalence Survey (2019-21) indicated that 42.6% of TB cases were detected through chest X-rays that might have been missed otherwise.
- Case Study: In rural Bihar, delayed diagnosis was identified as a primary reason for the continued spread of TB in certain high-burden areas.
Social Stigma and Economic Barriers:
- Challenge: TB patients often face social stigma, leading to delayed seeking of treatment. Additionally, the economic burden of TB treatment forces many families into poverty.
- Example: TB patients in urban slums often hide their condition due to fear of social ostracization, which results in advanced-stage diagnosis and poor outcomes.
- Case Study: In a Delhi slum, a survey revealed that 70% of TB patients had delayed treatment due to fear of losing their jobs, exacerbating their health and economic conditions.
Inadequate Healthcare Infrastructure:
- Challenge: Limited healthcare infrastructure, especially in rural and remote areas, hampers the timely diagnosis and treatment of TB.
- Example: Only 35% of Primary Health Centres (PHCS) in rural India have functional diagnostic equipment for TB, leading to under-diagnosis and under-reporting.
- Case Study: In a village in Madhya Pradesh, a lack of diagnostic facilities led to an outbreak of TB, affecting over 150 people within six months.
Co-Morbidities and Vulnerable Populations:
- Challenge: TB often affects vulnerable populations with co-morbidities like malnutrition, diabetes, and HIV, complicating treatment and increasing mortality.
- Example: India has a significant number of TB patients with diabetes, which worsens the prognosis and complicates treatment.
- Case Study: A study in Tamil Nadu found that 30% of TB patients with diabetes had a higher rate of treatment failure due to complications arising from both conditions.
Lack of Awareness and Behavioural Issues:
- Challenge: A lack of awareness about TB symptoms and preventive measures contributes to its spread. Behavioural issues, such as non-compliance with treatment, further aggravate the problem.
- Example: A survey in Uttar Pradesh revealed that 60% of the population could not identify TB symptoms, leading to delayed diagnosis and treatment.
- Case Study: In West Bengal, a study found that 40% of patients defaulted on their treatment due to a lack of understanding of the importance of completing the full course of medication.
Advancing Healthcare Initiatives at the Emerging Health Threats LIke Mpox & Cov-19
STRATEGIES FOR A MORE EFFECTIVE RESPONSE

Adopting Shorter, Effective Regimens for DR-TB:
- Strategy: Implementing the WHO-recommended shorter BPaL/M regimen for DRTB can improve treatment compliance and outcomes.
- Example: The introduction of BPAL/M regimens in several countries has shown a success rate of 89%, compared to the 68% success rate with older regimens.
- Case Study: South Africa’s roll-out of the BPaL/M regimen led to a significant reduction in DR-TB cases, with over 85% of patients completing the treatment.
Strengthening Diagnostic Infrastructure:
- Strategy: Expanding the use of rapid molecular tests and AI-driven chest X-ray machines can reduce diagnostic delays and improve case detection.
- Example: The use of GeneXpert machines in India has improved the detection of TB and drug resistance, leading to faster treatment initiation.
- Case Study: In a pilot project in Karnataka, the introduction of portable X-ray machines and rapid testing reduced the average diagnosis time from 45 days to just 10 days.
Community-Based Screening and Awareness Campaigns:
- Strategy: Conducting targeted, community-based screening drives, especially in high-risk populations, can detect TB cases early.
- Example: The ‘TB Mukt Bharat Abhiyan’ initiative focuses on door-to-door screening in slums, prisons, and other vulnerable communities.
- Case Study: In Maharashtra, a community-based TB screening drive led to a 20% increase in the detection of new TB cases within six months.
Enhancing Social Support Systems for TB Patients:
- Strategy: Providing social and economic support to TB patients, including nutritional support, counselling, and job protection, can improve treatment adherence.
- Example: The Nikshay Poshan Yojana provides a monthly nutritional allowance to TB patients, improving treatment outcomes.
- Case Study: A study in Jharkhand showed that patients receiving nutritional support under the Nikshay Poshan Yojana were 30% more likely to complete their treatment.
Leveraging Technology for TB Surveillance and Management:
- Strategy: Using technology such as GIS mapping and electronic health records can help in tracking TB cases, monitoring treatment, and identifying high-risk areas.
- Example: The use of eNikshay, an electronic platform for TB surveillance, has improved case tracking and reporting across India.
- Case Study: In Kerala, the integration of eNikshay with GIS mapping helped identify TB hotspots, leading to focused intervention and a reduction in cases by 15%.
Strengthening Political Commitment and Multi-Sectoral Collaboration:
- Strategy: Sustained political commitment and collaboration across sectors (health, nutrition, sanitation) are crucial for TB elimination.
- Example: The TB Free India campaign, supported by the Ministry of Health and Family Welfare, aims to eliminate TB by 2025 through a multi-sectoral approach.
- Case Study: In Tamil Nadu, a coordinated effort between the health and nutrition departments led to a significant reduction in TB cases among malnourished children.
Conclusion
- India’s multifaceted approach to combating tuberculosis showcases significant progress, with a 16% decline in new TB cases and an 18% reduction in mortality since 2015. However, challenges remain, necessitating sustained efforts and innovative strategies.
- The government must continue to leverage community support, enhance diagnostic capabilities, and address social determinants of health to achieve the ambitious goal of TB elimination by 2025.
- With ongoing commitment and collaboration among stakeholders, India can pave the way for a TB-free future, ultimately improving public health outcomes and economic stability